End of a Chapter
I have a few more hours to go before I'm done and rid of the ICU. But I spent a great deal of time today reflecting.
One, on rounds, reflecting on the miracles (and curse) of modern medicine, of the amazing technology we have that allows us to help the very sick. Airlift helicopters that bring patients directly to our hospital. The most modern of ICU medications or protocols that as far as I know are not yet available in Malaysia (activated protein C for sepsis, hydrocortisone infusion for severe pneumonia). Out-of-this-world gadgets (HFO: high frequency oscillator which ventilates ARDS patients with ultrahigh respiratory rates. This one lady is being ventilated with 300 breaths a minutes, with baby breaths!!). The curse is, with our abilities we sometimes prolong death when there is no more life to sustain. Case in mind, when an elderly lady coded at 230am today with no electrical rhythm (asystole, notoriously difficult to bring back) we resuscitated her for 10 minutes until someone shouted back, "Pulses!". She was transferred to the ICU where I took over care. When she was being wheeled to my unit, all of us doctors were feeling pretty good about ourselves, almost to the extent of high-fiveing each other for bringing her back. Until I did a thorough exam on her in the ICU. Fixed dilated pupils, no gag, blink or doll's eye reflexes. In other words, she was probably brain dead, and our medical know-how allowed us to bring her back despite that. Just before I left the ICU for good, I had a talk with her family and suggested we withdraw support.
Also did a lot of reflecting on my residency. Tonight was our official senior graduation dinner; I was able to leave the ICU for 5 hours to attend that. One realizes that this place holds a lot of memories, good as well as bad. Many good friendships that were fostered. And, despite where we all go, how our paths diverge, friendships that will last a lifetime. And no matter what happens, nothing can change the fact that we were trained at Mayo. That was in our program director's speech. True.
Officially, residency has another 2 months. But, our graduation dinner has come and gone. Internal Medicine, Class of 2005.

Henry, Rachel and I. Enjoying a pre-banquet cocktail.
Group photo, some of my classmates and I.

Dinner at the banquet hall, Foundation House
Wednesday, April 27, 2005
MICU
This is my team. Or at least part of it, some people were missing from the picture. We were mostly in good spirits, mainly because the month is coming to an end (although I have been pulled to cover the ICU for a week in June for someone). 3 more days in the MICU, woo hoo! Hmm, then again, I am on terminal call Friday night (also the night of the senior graduation dinner) so I hope I didn't just jinx myself.
Tuesday, April 26, 2005
Drained...
Sunday, April 24, 2005

Spent Saturday in Minneapolis with some friends. Did some shopping at Ikea... splurged on beddings and stuff, things I don't normally fuss on. But my comforter was starting to fall apart, and I decided to spoil myself for once with something else other than electronics.
It was a great day. Good time with good friends, and good music. Dim Sum lunch, and then a nice rib dinner with a good band. Got back past 10pm, but it was a good day.
Friday, April 22, 2005
Tuesday, April 19, 2005
Things You Don't Wanna Hear Your Doctor Say
- Oops!
- Oh Crap! (actually uttered those words when I was putting a line into the internal jugular last week. Luckily the patient didn't hear me)
- By the way, you weren't planning on having more kids were you?
- Are you insured?
- My name is Dr. Hannibal Lecter
- Nurse, we're gonna need the heavy-duty cement-dissolving enema
- You did say you were here for a vasectomy, didn't you?
- First, lemme give you the good news....
- Are we missing a pair of surgical forceps?
- You win some, you lose some
- Humming the tune of Money, Money, Money when he's checking you out
- I'll need the larger gauge needle
Monday, April 18, 2005
Thursday, April 14, 2005
The Definition of Irony
- Medical staff watching an episode of ER in the ICU
- A mechanically-ventilated patient with endstage alcoholic liver disease, whose first words when regained consciousness were 'Give me alcohol...'
It was a busy call again last night, partially too thanks to the incompetence of the ER. Received at least one bogus ICU admission, who really didn't even needed to be in the hospital. 'Pneumonia' in the context of a normal white cell count, no fever, unchanged chest X-ray and normal O2 saturation. Really. While I don't consider myself smart (conversely, I think my IQ is pretty low) at least I'm not in the habit of taking shortcuts and blocking admssions of every Jane or Joe who comes in. I was pretty miffed with the Pulmonary resident (a junior of mine) who declined to accept the patient and insisted on her coming into the ICU, just so he could get extra sleep and not work her up. Out of sheer laziness, and without even looking at the chest Xray he just said no, too 'unstable' for the floor.
But the others though, were sick. We usually worked as a team, my fellow, intern and I. But last night we had several patients arrive and crash at the same time, so we had to tag-team. Last night itself I had to intubate one patient and place 3 central lines in others.
I was able to finally lie down for a 45 minute quickie nap at 4am, 21 hours after starting call. By then, my brain had stopped working and I really just couldn't care less about anything else except getting sleep. Until I got the call that a patient's BP was 60/30.
Tuesday, April 12, 2005
He'll probably pass on tonight. Not in any pain or suffering, I hope. I told his nurse to give him as much morphine as he needs to be comfortable. Everyone understood what that meant. Even if it means that that stops his breathing.
Monday, April 11, 2005

Honda S2000.
My new car.
Heh heh, I wish.
Took Veronica to the mechanic's today (had the day off) for an oil change. Since it would take 45 minutes, the Honda people let me take their S2000 out for a spin. They know me, and I had brought them some friends who ultimately bought cars from them. So they were particularly nice to me.


Sunday, April 10, 2005
Sushi

My version of sushi. This is kinda backdated; did this last weekend. Was able to find a lot of sushi ingredients here (surprising, considering the size of this city). Anyway, it turned out quite well, and I was able to appease my lust for sushi (for now at least).
Friday, April 08, 2005
No Problem!

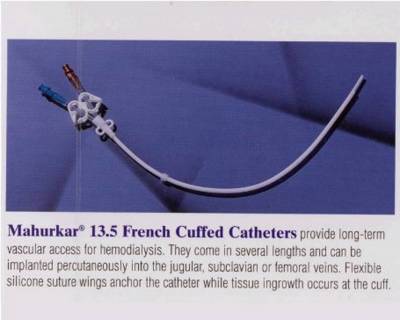
"Size 7 1/2 gloves please. "
My critical care fellow stood beside me, providing back-up. My intern had declined to perform the procedure.
Looking at Mr. B now, I can't blame her. He's morbidly obese, over 300 lbs. I wonder how someone can allow themselve to get like this. Worse of all, he practically had no neck. So much for looking for the apex of the sternocleidomastoid.
We'll need the site-rite.
I guided the 'poor man's ultrasound' probe to his right neck. There! Didn't seem that difficult to find his internal jugular. Compressible? Check. That's not his carotid (good thing).
I scrubbed and gowned up. The patient, already intubated and on a vent, was unaware of my presence and what I was going to do to him (his next-of-kin, of course, had consented).
After infiltrating the skin with lidocaine (not necessary, really, since he was out. But habits die hard), I took the 3 1/2 inch gigantoid needle, and stuck it into his neck at a 45 degree angle. First go, no aspirate. Partial withdraw and aimed more laterally and went in again, while pulling on the plunger of the syringe. No blood. Repeated 3rd, 4th time (why oh why did I volunteer to insert a central line into the biggest patient we had in the ICU?). On my fifth try... about 2 inches in (I was starting to worry about popping his lung)... flashback! Nice aspirate of dark, venous blood. Removed the syringe and confirmed it wasn't the carotid (it wasn't squirting into my face). Quickly inserted the guidewire, then made a cut with the blade, and then the dilator. Finally, shoved in the dialysis Mahurkar line as far in as it would go. Put 2 stitches in, and I was done.
Good work, my fellow said.
No problem, I lied.
Thursday, April 07, 2005
10 Things I Want to do Before I Die
Mrs. B, the lady we admitted the other day with metastatic non-small cell lung cancer and septic shock, was extubated yesterday. She's talking now. Told us she wasn't ready to die; there were things she wanted to do still.
Well, what about me? What would be on my to-do list, before I kick the eternal bucket?
- Skydive
- To find my soulmate, and marry her (just once in this lifetime, mind you. Not the Britney marry-one-day, annul-the-next type)
- Raise a family
- See my grandkids
- To see my sis take the Hippocratic Oath
- Visit Australia
- Get a tattoo on my right arm
 (Have been talking about this for 4 years, doubt I'd ever find the guts to do it. Mom's threatened to disown me!)
(Have been talking about this for 4 years, doubt I'd ever find the guts to do it. Mom's threatened to disown me!) - Go on a Caribbean cruise
- Drive a convertible
- Write a book (a real book, not a textbook)
Wednesday, April 06, 2005
Finally!
I will keep you updated on any other information I get from them including target publication date and formal title of the book so that you can add your chapter to your CV.
Thanks again for your important contribution - I think you will be pleased with the company that each of your chapters will keep inside this volume. "
Morally, perhaps this may be wrong, letting someone go. But, I wonder if all these 'pro-life' people know what it means to be in a persistent vegetative state? Yes, it sounds nice, keeping someone alive. But have they seen the massive pressure ulcers people get just lying in bed, the ones that are so deep that you see pelvic/hip bone? The complications of being bedbound? Of tube feeding?
Tuesday, April 05, 2005
Monday, April 04, 2005
Medical ICU
Sunday, April 03, 2005
Sun!

Finally! After waiting for months, was able to take my bike out out of garage for biking. 21-speed front & rear suspension Mongoose. Had neglected him for a while now. But Sunday was just so sunny that I couldb't resist. A high of 18C! Gawd, how I miss biking. Hopefully, it'll be warm enough in the next month for us to go canoeing.
I think we've seen the last of snow, at least till next winter. In fact, the days were so nice that I went out and bought a Black & Decker high pressure washer for my car, and gave her a nice 2 hour wash and wax. I think I need to get a life!


